Even after childhood cancer treatment is over, survivors often continue to experience significant health effects. Approximately 95% of childhood cancer survivors will incur at least one health-related issue in their lifetime. Complications, disabilities, or adverse outcomes from chemotherapy, radiation therapy, and/or surgery often continue the need for medical intervention and monitoring for childhood cancer survivors. Survivors should continue meeting with their medical team after treatment, and transition to a survivor’s clinic when recommended.
Late effects may include: cognitive impairment; fertility problems; alterations in growth and development; organ system damage; chronic hepatitis; and secondary cancers. Survivors frequently have more than one late effect, with perhaps as many as one-third of survivors experiencing one that is severe or life-threatening. Survivors and their families can lower potential risk by educating themselves on what to look for and how to proceed with the recommended follow-up plan.
A childhood cancer survivor’s quality of life is a spectrum. Some survivors are living life with little to no impact, while others experience a heavy burden of late effects. Some treatment side effects continue after treatment and may disappear with time. Other late effects can develop a few years post-treatment, during puberty, or much later in adulthood. This section provides answers to common questions and details the broad spectrum of health complications survivors may face during their lifetime. No survivor experiences all of these complications, but rather individual late effects result from the combination of genetic predisposition and the huge variance of treatment options available for childhood cancers. It is often helpful to refer to the side effects that are typical with a childhood cancer diagnosis and treatment to identify the side effects that could potentially develop during survivorship. Families can work with their team to determine risk and vulnerability, and to evaluate symptoms.

Transitioning from treatment and embracing the new journey of childhood cancer survivorship can pose significant physical and emotional challenges. During treatment, patients are constantly monitored by medical experts, often in a hospital setting. When treatment ends, patients return home and can no longer rely on regular evaluations or basic symptom monitoring by their care team. The loss of the customary routines and oversight can instill fear in parents, caregivers, families, and even survivors who had actively participated in discussions and decision making. Agreeing on a survivorship plan and collaborating with a supportive medical team can help smooth the transition. Survivors and their families should become familiar with critical aspects of their situation, and organize the important details of the treatment process for their records. For parents, and survivors as they grow up, it is important to learn how to continue to effectively monitor symptoms and collaborate with medical experts to manage post-treatment side effects and chronic health issues.







Learn more about a child’s vulnerability to developing post-treatment side effects throughout the life span. Puberty and continued development in adulthood can bring about changes in late effects, resulting in revisiting side effects that had disappeared, exacerbating issues and making them worse, and developing new issues. Unfortunately, the survivorship journey may include the development of subsequent cancers and coping with chronic pain. Learn more about the risk of developing secondary cancers related to childhood cancer treatment; the evaluation and management of chronic pain associated with a wide array of side effects; and how a child’s genetics and hereditary factors can influence the development of certain long-term effects.





The nervous system is composed of the brain, spinal cord, and a complex network of nerves. The brain controls all of the body’s functions, and the hallmark of this system is sending messages to and from the brain and the spinal cord to various parts of the body. When these nerves function properly, each organ system can communicate with and between each other. Sometimes, treatment permanently affects childhood cancer patients’ nervous systems. One key area to monitor is the sensory system that includes the five senses: hear, smell, taste, touch, and vision. Depending on the type of childhood cancer and the treatment received, survivors often deal with partial or total loss of sight or sound, and modifications in smell, taste, and touch. Given the complexity of these issues and their importance to nervous system functioning, using a holistic, multi-pronged approach helps keep appropriate attention on this crucial system.







Whether immediately after treatment or decades later, childhood cancer treatments often affect the heart, veins, and arteries. It is crucial for survivors to undergo annual evaluations with a cardiac doctor who can attend to their complete cardiovascular system and address recommended screening guidelines. If there is an issue with the heart or surrounding blood vessels, early detection helps to minimize the negative impact on survivors.






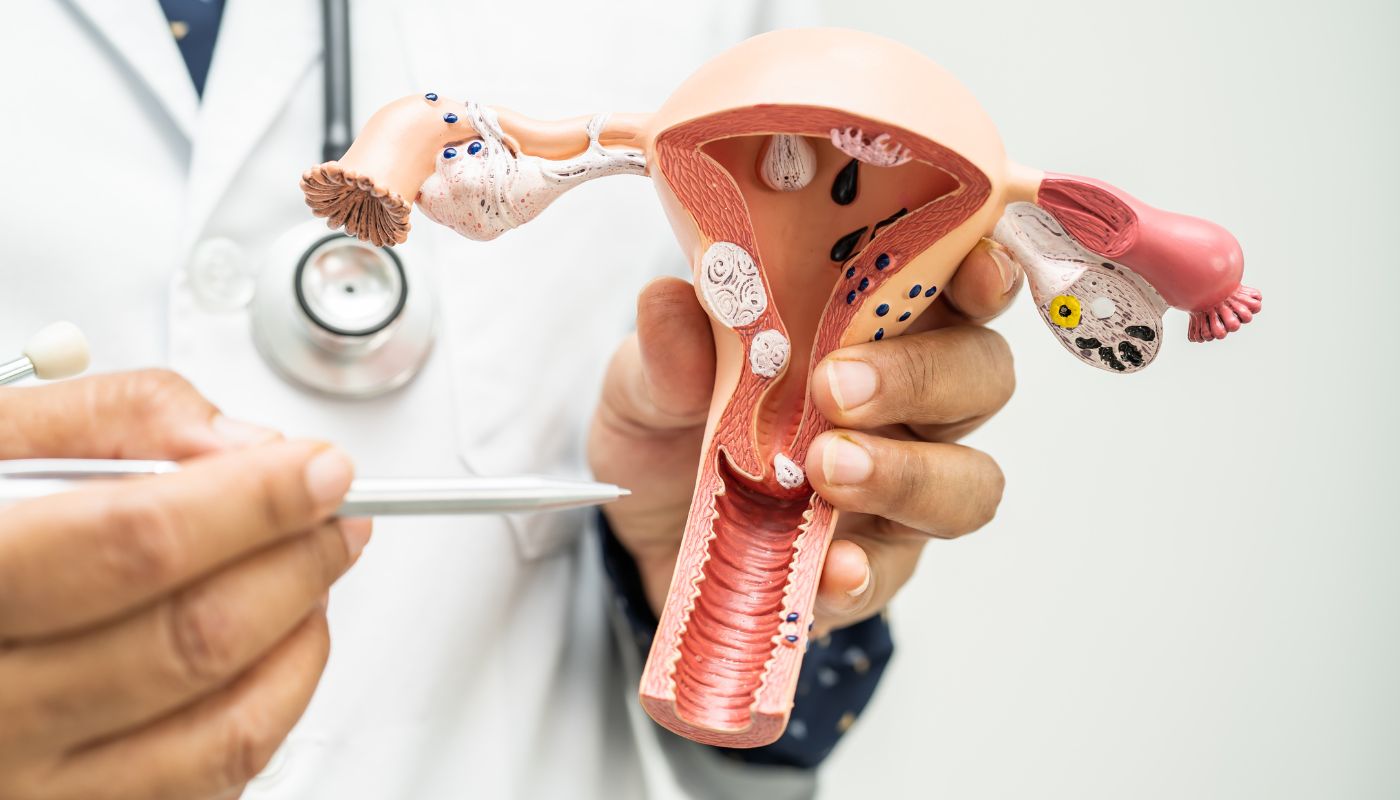
For childhood cancer survivors, fertility and hormonal health related to sexual development can raise sensitive challenges. Cancer treatment can harm sexual health and ability. Females may struggle with ovarian and uterine function, and face challenges getting pregnant and/or carrying a child full term. Males may struggle with sexual dysfunction, erectile dysfunction, or fertility. Any survivor can experience emotional distress related to these issues. Learn more about the problems that childhood cancer survivors may face, and support available to them.






The digestive system encompasses the entire process of breaking down food to absorb nutrients and sustain the daily functions of the human body. It includes oral and dental components, and the esophagus, stomach, liver, gallbladder, pancreas, and the small and large intestines. Children undergoing cancer treatment often face various challenges due to chemotherapy, radiation, or surgery, which may persist even after treatment. It is essential to understand these issues, detect them early, and learn ways to prevent or minimize symptoms.








The skeleton, which includes bones, ligaments, tendons, cartilage, joints, and other connective tissues, as well as the muscles attached to it, create the musculoskeletal system. The primary function of this system is to support and move the body. In addition, the musculoskeletal system provides protection, generates heat to maintain the body’s temperature, and aids in blood circulation. There are several late effects that childhood cancer survivors may experience related to the musculoskeletal system. Survivors should pay attention to various elements of bone health, such as preventing osteoporosis and osteopenia. Osteosarcoma survivors often must manage limb loss/salvage surgeries, amputations, and prosthetics. Radiation to the spine during treatment may also mean that the survivor should monitor for spinal deformities of scoliosis, kyphosis, and/or lordosis.





The respiratory system includes the lungs, nose, mouth, throat, voice box/larynx, and the windpipe/trachea. The respiratory system’s primary function is to breathe, allowing the body to absorb oxygen and remove carbon dioxide from your blood for optimal functioning. Often, childhood cancer survivors must contend with various respiratory diseases and difficulties throughout the duration of their lives. Some of the more common respiratory issues include asthma, pulmonary fibrosis, and restrictive lung disease.







The endocrine system consists of a network of glands and organs using hormones to communicate between two parts of the body. That system also controls the body’s metabolism, growth and development, energy levels, reproduction processes, and helps in the body’s response to injury, stress, and mood. The major endocrine glands in the human body are the thyroid, parathyroid, pituitary, pineal, and adrenal glands. Childhood cancer survivors often face various complications with their endocrine system. Both chemotherapy and radiation can result in growth hormone deficiencies for survivors. In addition, childhood cancer survivors may face various difficulties with the immune and lymphatic systems throughout survivorship. The immune system protects the body from various diseases by detecting and responding to anything different than the body’s healthy tissue, such as viruses, parasites, and cancer cells. The lymphatic system is part of the immune system and complementary to the circulatory system. It consists of an extensive network of lymphatic vessels, nodes, organs, tissues, and lymph that help with immune defenses. Both systems can be disrupted by treatments.








The renal system consists of the kidney, ureters, and the urethra. The kidneys filter the blood for waste, and then create urine to excrete the waste. The kidneys, however, have many other functions, including: balancing the body’s fluids; releasing hormones that regulate the body’s temperature; producing active vitamin D for strong, healthy bones; and controlling red blood cell production. Once the kidneys create the urine, it travels through the ureters, one for each kidney, and then to the bladder, where it is stored until expelled. The urinary system also regulates blood pressure and blood volume in the body. It also controls levels of electrolytes and metabolites, and regulates blood pH. Chemotherapy medications and surgery can harm the kidneys, either resulting in the removal of one kidney, or compromising one or both kidneys.







The aftertaste of the childhood cancer treatment experience is the fear that cancer will return. Whether it is a recurrence or a second diagnosis, childhood cancer survivors and families worry about a day when they will hear that their worst fears are confirmed. What are the risks and concerns at such a time? These resources address the important considerations when discussing recurrence or new cancer diagnoses.




The Children’s Oncology Group recommends that every family receive and maintain a complete summary of their child’s cancer treatment: “The survivor or their parents should ask for a treatment summary from the hospital or clinic where they received their cancer treatment. The treatment summary should be kept in a safe place, and a copy should be given to all healthcare providers involved in the survivor’s care (for example, your family doctor, your pediatrician, any specialists).”
A Cancer Treatment Summary should contain the following information:
Children, adolescents, and young adults surviving childhood cancer require ongoing, specialized care and follow-up. Sometimes survivorship clinic care is provided by medical professionals who were part of the treatment team. Other times a survivorship clinic may be better equipped to monitor late effects and follow survivorship plans. Some survivorship clinics set age limits of 21 years, while others provide care throughout the survivor’s life. Discussing the survivorship clinic options with your medical team to determine if your child will need to transition to an adult clinic at some point in the future is crucial.
Cancer survivors who have had radiation therapy can be more susceptible to skin cancer. Chemotherapies like Adriamycin and daunorubicin can also make cancer survivors more susceptible to skin cancers. Some survivors can have significant radiation recall, causing excessive burns when exposed to the sun, even long after therapy is over.
LEARN MORE
Survivors should be able to participate in sports to the best of their abilities. Understanding the potential late effects and how they may impact exercise and participation in certain sports activities is crucial. For example, vision or hearing loss can affect the ability to play certain sports. Additionally, kidney damage or the development of cardiomyopathy may limit specific sports options. Get clearance to play by seeing a pediatrician or adolescent care physician who will complete the necessary athletic forms, and discuss any potential risks. Remember to take the necessary precautions to protect vulnerable organs. For instance, if you only have one kidney it is recommended to avoid high-impact sports like football or lacrosse. Consider discussing any late effects with your school nurse or trainer, so they know your background in the case of any potential emergencies.
Some digestive issues may persist after cancer treatment, but they often improve over time and eventually disappear. Some survivors however may continue to experience significant gut health challenges as they age. Gut health refers to the efficient digestion and absorption of food. These challenges may arise because of changes to the gut biome that result from exposure to chemotherapy or antibiotics, or due to issues in the neuromuscular innervation. Many of these conditions can be managed with medications or dietary changes. To find the right approach, consider seeking help from a medical professional.
LEARN MORE
Many survivors can become parents; however, this largely depends on the types of cancer and treatments received. Both male and female survivors may experience fertility issues. Additionally, some survivors may find that they should consider other late effects, such as heart conditions, when deciding to have children. As children mature, discuss these issues with them on an age or developmentally-appropriate level during annual evaluations at the Survivorship Clinic, and at home when it is of interest or concern to your child.
LEARN MORE
Excessive weight gain may result from changes in the ability to regulate sugar or other endocrine hormones due to chemotherapy or radiation. Special tests can measure hormone levels, such as cortisol or insulin, and how they respond to eating or fasting. It is crucial to discuss these concerns with your pediatrician or adolescent care physician, as well as your survivorship clinic team. Childhood cancer survivors are at a significantly higher risk of developing obesity and cardiometabolic conditions.
LEARN MORE