By CAC2 Member Susan Guisto (Friends of Cathryn Foundation) and Guest Blogger Judith G. Villablance, MD, Children’s Hospital Los Angeles Every year, approximately 1 in 10,500 children from birth to 15 years of age are diagnosed with cancer in the United States. Most pediatricians will likely encounter only one to three cases throughout their professional lifetime. Even though a pediatrician may never see a case of cancer in his or her practice, it is important to understand what to look for, how to evaluate patients and to ensure follow-up and timely referrals to specialists. As a result, pediatricians can play a critical role in minimizing delayed diagnoses to give patients the best possible outcomes. For any pediatric cancer, patients may not present with the classically described symptoms. This was supported by a 2020 survey of 300 parents in the U.S. who had a child or a young adult who was diagnosed with high-risk neuroblastoma, including survivors and angels (S. Giusto). The most common initial complaints were leg pain/refusal to walk, persistent low-grade fever or unexplained fever spikes, fatigue, anorexia, constipation, and changes in mood/behavior—all of which may not have been apparent during office visits. This underscores that non- specific symptoms can indicate neuroblastoma, and parent observations are an important diagnostic tool. This is illustrated by the story of a child ultimately diagnosed with metastatic high-risk neuroblastoma from the mother’s perspective: “Our healthy 4-year-old daughter spontaneously spiked a 105F fever and began to complain of headaches and fatigue. The pediatrician considered these issues ‘random and not concerning, perhaps due to not getting enough water or sleep’. The following few weeks, we noticed temperament changes and frequent complaints of back pain. The pediatrician ruled out scoliosis, considered the symptoms growing pains and no follow- up or referral was suggested. We requested an X-ray of my daughter’s back and were told it wasn’t necessary because pediatricians want to avoid unnecessary radiation. In ensuing weeks, symptoms, including frequent backaches, continued intermittently; our daughter mentioned that it really hurt her back when I hugged her. We insisted on a specific X-ray where the pain was isolated in her back, which revealed a large paraspinal mass, exactly where she had said it hurt. We were immediately sent to a children’s hospital spine specialist who looked at the X- ray and proclaimed it to be a tumor, in all likelihood cancer. We would soon learn that it was stage 4 neuroblastoma and had spread throughout her body, skull, and bone marrow. From first appointment to diagnosis was 7 months.”
Factors impacting time to diagnosis: The figure below illustrates the Children’s Cancer Diagnosis Pathway (1,2) and demonstrates that diagnosis delays can be subdivided into two components—time from symptoms onset to first health care contact (Patient Delay) and time from that event to diagnosis (Physician Delay). It also lists contributing factors (1).
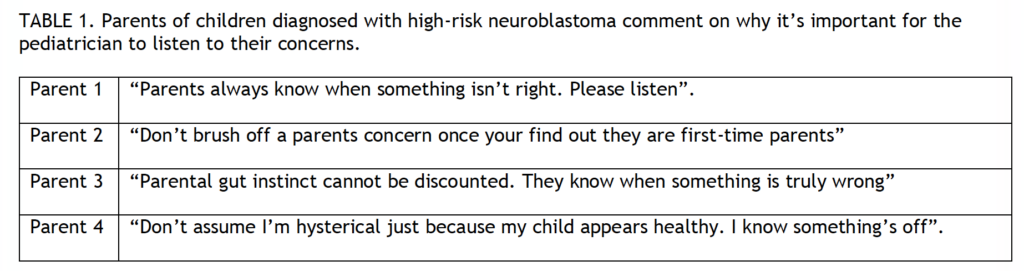
Opportunities to Improve Time to Diagnosis A key component for determining any pediatric diagnosis is to listen to parents. Their intuition and observations of their child’s temperament and subtle health changes not evident during office visits are important clues. Pediatricians can optimize making the right diagnosis by validating parental concerns and scheduling follow-up for patients with non-specific symptoms. A survey of parents of 58 children with high-risk neuroblastoma illustrates this point (S. Giusto) (Figure 2).
Diagnostic delays may be improved with targeted programs. The HeadSmart program, a web-based national awareness campaign in the United Kingdom decreased time to diagnosis for pediatric brain tumors by half (3). HeadSmart included partnering with parents via “safety netting.” When symptoms did not lead to an immediate diagnosis, plans were made with the patient/parent about next steps if the problem did not resolve. This included return visits within a given time and specialist referrals if symptoms persisted or worsened.
ChildCancerSmart is an ongoing successor project that aims to reduce time to diagnosis for all cancers in children, adolescents, and young adults. ChildCancerSmart is a public/professional education program on symptoms of childhood cancers and promotes partnerships with parents that prioritize parental concerns. It includes a quarterly publication, called Contact, for children’s cancer parent and physician communities. Contact includes stories of diagnoses, survival, medical advancements, and treatment focused on childhood and adolescent cancer. Dr. Scott Coven (University of Indiana) is developing a program based on HeadSmart to improve recognition of brain cancer symptoms among United States pediatricians (4). He believes “a child’s journey with cancer starts well before the diagnosis. It is imperative that we (as providers) intently listen and validate caregivers’ concerns as they encounter the health care system. Striving for a timelier diagnosis can be a goal that unites caregivers, primary care providers and pediatric oncologists. If we fail to build a strong patient-provider relationship prior to diagnosis, the distrust for health care professionals will likely persist long after treatment is completed.” While the impact of delayed diagnosis of pediatric cancers on outcome is variable and not well defined (1,3), delays can impact parent/patient trust in the setting of a potentially life-threatening disease. In summary, it is crucial for pediatricians to listen to parents, validate their concerns and follow up on symptoms that appear benign but do not resolve. It is also important to access pediatric cancer specialists to discuss when further workup is indicated. The trust between a parent and pediatrician is significant. One of the most important decisions a parent makes is choosing the pediatrician for their child. Pediatricians can earn and repay that trust by following the simple suggestions in this article. Further studies defining causes of diagnosis delays and effective interventions are needed.References