Childhood Cancer Fact Library
Supported by SebastianStrong Foundation.
A comprehensive, well-documented and trusted source of information for anyone seeking data and statistics related to pediatric cancers. The Fact Library team updates its listing annually so that it can continue to be instrumental in building awareness of the realities associated with diagnosis, treatment, remission, and survivorship.
LATEST COMPLETE DATA YEAR: 2022 (Please note: Data is compiled each year and released at the end. 2023’s data will come next year. 2022 is the most current data available.)
All statistics below are for U.S. children from birth through age 19 unless stated otherwise. This summary relies on the most recent published data with respect to its contents, some of which dates back one or more years.
Find supporting graphics from the Childhood Cancer Fact Library
Diagnosis
- Childhood cancer is not one disease – there are more than 12 major types of pediatric cancers and over 100 subtypes. (1)
- In 2023, it is estimated 9,910 children (birth to 14 years) and 5,280 adolescents (aged 15-19 years) will be diagnosed with cancer. (1A)
- The overall incidence of childhood cancer is on the increase, averaging 0.8% increase per year since 1975. Children (0-14) increased 0.8%, and adolescents also increased 0.8%. Overall cancer incidence rates increased an average of 1% per year from 1997 to 2018. (45A) Among children aged 0-14, the incidence rate for all cancer sites combined was 17.8 cases per 100,000 persons. Among AYAs, the overall cancer incidence rate was 77.9 cases per 100,000 persons. (7G)
- In 2022, there were approximately 87,050 cancer cases diagnosed and about 9,180 cancer deaths in adolescents and young adults (AYAs) ages 15 to 39 years in the US. (40)
- About 1 in 260 children will develop cancer before the age of 20. (1a)
- Children with Down syndrome are 10 to 20 times more likely to develop leukemia than children without Down syndrome. (37)
- 47 children per day or 17,293 children (aged 0-19) were diagnosed with cancer in 2018.(45)
- As of 2018, 4,317 children and teens under age 20 were diagnosed with CNS tumors, accounting for 25% of total cancer diagnoses in the age group 0-19. (45)
- Approximately 8% of all newly diagnosed brain tumors occur under age 20 (67)
- The average age at diagnosis is 10 overall (ages 0 to 19), 6 years old for children (aged 0 to 14), and 17 years old for adolescents (aged 15 to 19)(9), while adults’ median age for cancer diagnosis is 66 (7a)
- Most new cancer diagnoses in children are for leukemia (28.1%) and brain/CNS cancers (26.5%), while malignant epithelial neoplasms and melanomas (23.3%) and brain/CNS cancers (21.9%) are top cancers for adolescents. (45)
- The most common cancer types among children (0-14) included leukemia, brain and other nervous system, and lymphoma, with cases increasing by 0.7% – 0.9% per year on average for all three during 2001-2018. (7G)
Long Term Health-Effects Associated with Treatments & Survival
- Cancer treatments may harm the body’s organs, tissues, or bones and cause health problems later in life. These health problems are called late effects as a result of surgery, chemotherapy, radiation therapy, and/or stem cell transplant. Late effects in childhood cancer survivors affect the body and mind. Late effects may affect organs, tissues, body function, growth and development. Other late affects are mood, feelings and actions thinking, learning, and memory as well as social and psychological adjustment. Late effects also have a risk of second cancers. (39)
- The chance of having late effects increases over time. New treatments for childhood cancer have decreased the number of deaths from the primary cancer. Because childhood cancer survivors are living longer, they are having more late effects after cancer treatment. Survivors may not live as long as people who did not have cancer. The most common causes of death in childhood cancer survivors are: The primary cancer comes back or a second (different) primary cancer forms or there is heart and lung damage. (39)
- Childhood cancer survivors who received radiation or certain types of chemotherapy have an increased risk of late effects to the heart and blood vessels and related health problems. (39)
- NCI researchers observed that children who received radiotherapy had an increased risk of developing meningioma, cancer of the membranes that surround the brain and spinal cord (meninges).(72)
- Long-term follow-up analysis of a cohortof survivors of childhood cancer treated between 1970 and 1986 has shown that these survivors remain at risk of complications and premature death as they age, with more than half of them having experienced a severe or disabling complication or even death by the time they reach age 50 years. (63).
- Children and adolescents treated in more recent decades (after 1986) may have lower risks of late effects due to modifications in treatment regimens to reduce exposure to radiotherapy and chemotherapy, increased efforts to detect late effects, and improvements in medical care for late effects. (63)
- More than 95% of childhood cancer survivors will have a significant health related issue by the time they are 45 years of age (2); these health related issues are side-effects of either the cancer or more commonly, the result of its treatment. 1/3 will suffer severe and chronic side effects; 1/3rd will suffer moderate to severe health problems; and 1/3rd will suffer slight to moderate side effects. (2)
- Cognitive impairment affects up to one-third of childhood cancer survivors. (38)
- A large follow-up study of pediatric cancer survivors found that almost 10% developed a second cancer (most commonly female breast, thyroid, and bone) over the 30-year period after the initial diagnosis. (38)
- Treatment for cancer may cause infertility in childhood cancer survivors. Infertility remains one of the most common and life-altering complications experienced by adults treated for cancer during childhood. (64)
- Having a bone marrow or stem cell transplant usually involves receiving high doses of chemo and sometimes radiation to the whole body before the procedure. In most cases, this permanently stops ovaries from releasing eggs, resulting in lifelong infertility.(66)
- Female childhood cancer survivors who were treated with chemotherapy— even if they did not receive radiation treatments to their chest — are six times more likely than the general population to be diagnosed with breast cancer later in life. For those who did receive chest radiation, that chance increases exponentially and is on par with those who have the BRCA1 or BRCA2 mutations. (28)
- Childhood cancer survivors are at a 15-fold increased risk of developing Congestive Heart Failure and are at 7-fold higher risk of premature death due to cardiac causes, when compared with the general population. There is a strong dose-dependent relation between anthracycline chemotherapy exposure and CHF risk, and the risk is higher among those exposed to chest radiation. (33)
- Children who were treated for bone cancer, brain tumors, and Hodgkin lymphoma, or who received radiation to their chest, abdomen, or pelvis, have the highest risk of serious late effects from their cancer treatment, including second cancers, joint replacement, hearing loss, and congestive heart failure. (4)
- Compared with the general population, survivors of childhood and adolescent cancers have an increased risk of 6 major psychiatric disorders, including: Autism spectrum disorder (hazard ratio [HR], 10.42), ADHD (HR, 6.59), PTSD (HR, 6.10), OCD (HR, 3.37), Major depressive disorder (HR, 1.88), Bipolar disorder (HR, 2.93). (62)
- Life expectancy for five -year childhood cancer survivors has steadily increased. Life expectancy for those treated in the 70’s is only 48.5 years and survivors treated in the 80’s have a life expectancy of 53.7 years, while those treated in the 90’s rose to 57.1 years. (41) Normal life expectancy for adults is 80. (13)
- Nearly a quarter of childhood cancer survivors experience at least one debilitating neuromuscular condition 20 years post diagnosis. (47)
Treatment, Research, Funding
- On average, in 2009 pediatric hospitalizations principally for cancer were 8 days longer and cost nearly 5 times as much as hospitalizations for other conditions (12.0 days versus 3.8 days; $40,400 versus $8,100 per stay). Costs per day were about 70 percent higher for pediatric cancer stays ($3,900 versus $2,300 per day). (5)
- In 2009, pediatric stays principally for cancer cost nearly one billion dollars, accounting for over 5 percent of pediatric non-newborn inpatient hospital costs. (5)
- One in four families lose more than 40% of their annual household income as a result of childhood cancer treatment-related work disruption, while one in three families face other work disruptions such as having to quit work or change jobs.
- 1 in 5 CHILDREN who receive a new diagnosis of childhood cancer are already living in poverty. (36)
- Parents of long-term childhood cancer survivors reported lower household income and higher risk-of-poverty. In a study group of 769 parents of long-term childhood cancer survivors, 30.4% reported lower household income and were at higher risk-of-poverty. (36a)
- More than 90% of children and adolescents who are diagnosed with cancer each year in the United States are cared for at a children’s cancer center that is affiliated with the NCI-supported Children’s Oncology Group(COG). Children’s Oncology Group is the world’s largest organization that performs clinical research to improve the care and treatment of children and adolescents with cancer. Each year, approximately 4,000 children who are diagnosed with cancer enroll in a COG-sponsored clinical trial. COG trials are sometimes open to individuals aged 29 years or even older when the type of cancer being studied is one that occurs in children, adolescents, and young adults. (4)
Funding
There are two conflicting reporting methods available that are used to gauge federal childhood cancer research investment. A report used in the past and often cited by advocates, is the National Cancer Institute’s Funded Research Portfolio (NFRP)(7C) below. It indicates that from 2008 through 2018, the NCI spent an average of 4.08% of its obligations on childhood cancer research. According to NCI’s Office of Advocacy Relations (OAR), the NFRP does not reflect NCI’s total investment in any one particular area of research—including childhood cancers—because it does not account for basic science awards, which are not categorized by cancer type and which may have applications to multiple types of cancer.
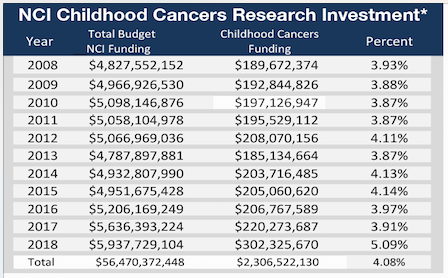
About the NCI Funded Research Portfolio (https://fundedresearch.cancer.gov/nciportfolio/)
The NCI Funded Research Portfolio (NFRP) web site contains information about research grants, contract awards, and intramural research projects funded by the National Cancer Institute. The NFRP provides access to various NCI budget reports that contain information about research funding according to specific research categories. It also provides the ability to search the database in
various ways, including text searching of project abstracts and the ability to search the NIH research categories that are assigned to projects carried out by extramural and intramural groups. (7D)
How does NCI generate NFRP funding data?
At the close of each fiscal year, NCI asks each of its scientific organizations to report their research funding according to specific research categories. The reports that NCI intramural and extramural programs provide are then combined to determine the NCI funding totals for individual research areas. The total research funding for each category is reviewed and verified before NCI publishes on the NCI web site, Cancer.gov. (7D) Unfortunately, the present NFRP only has been completed through 2018 and should have been completed through 2020.
What is scientific coding?
Scientific coding refers to the categorization of research projects according to scientific focus. In this process, research projects are analyzed and classified according to scientific topic and content. Scientific coding allows the development of science-based budget information, which can be used in portfolio analysis to examine the distribution of funds across research areas. Scientific coding is also necessary to answer inquiries about the scientific and budgetary aspects of Institute-funded research. NCI employs a sophisticated system of scientific coding in which trained professionals and/or scientific staff analyze grant applications, contracts, and intramural projects to classify each project for its degree of relevance to Special Interest Category (SIC) and Organ Site (SITE) codes. This coding structure is meant to describe in a consistent way the major scientific disciplines requested by NIH, DHHS, Congress, and the public. A critical characteristic of coded data is comparability from one fiscal year to the next. This process allows the Institute to respond quickly to requests for information from NCI staff and the broader community. The coding definitions used by the NCI intramural program are consistent with those used for extramural grants and research and development (R&D) contracts to maintain accuracy across the Institute’s portfolio. (7D)
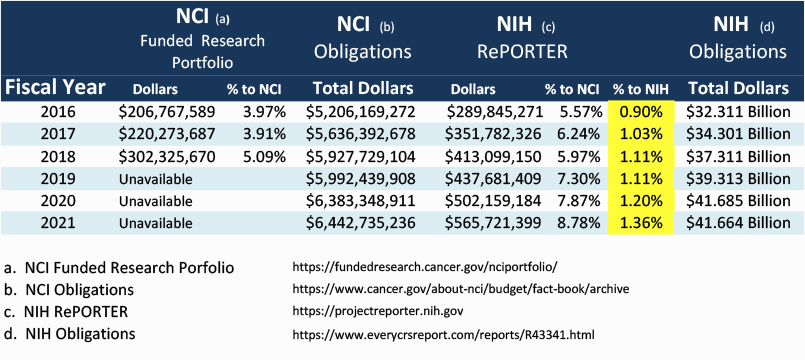
- Another report, preferred by OAR, is the NIH RePORTER, which is a congressionally mandated system all NIH Institutes and Centers (ICs) use to report data by fiscal year (FY). This tool highlights annual support for various research, condition, and disease categories (RCDC) based on grants, contracts, and other funding mechanisms used across NIH. Unlike the NFRP report, this method utilizes a word search program rather than scientific coding to determine category spending.
NIH RePORT Categorical Spending (RCDC) NCI – Pediatric Cancer Category
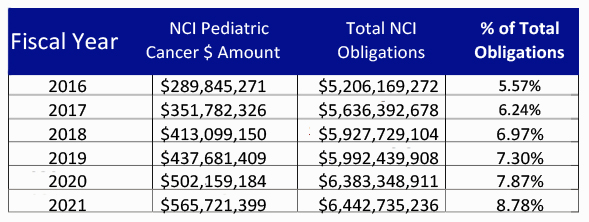
According to OAR, like the NFRP, the NIH RePORTER also does not account for the totality of NCI’s investment in a given area of research because basic science awards cannot be categorized by individual cancer type. Using Total NCI Obligations, without making allowances for NIH items included in the Pediatric Cancer Amount, would distort the percentage of Total Obligations.
While both of the above reports, The NFRP and the NIH RePORTER, seem unable to capture a completely accurate measure of childhood cancer research expenditure as it relates to total research dollars, perhaps a better method to measure progress may be to compare NIH RePORTER pediatric dollars (c) to the Total NIH Dollars (d) for each fiscal year. This method would show changes from one year to the next. Note that the chart below shows that the pediatric cancer expenditures are growing from 2016 to 2021.
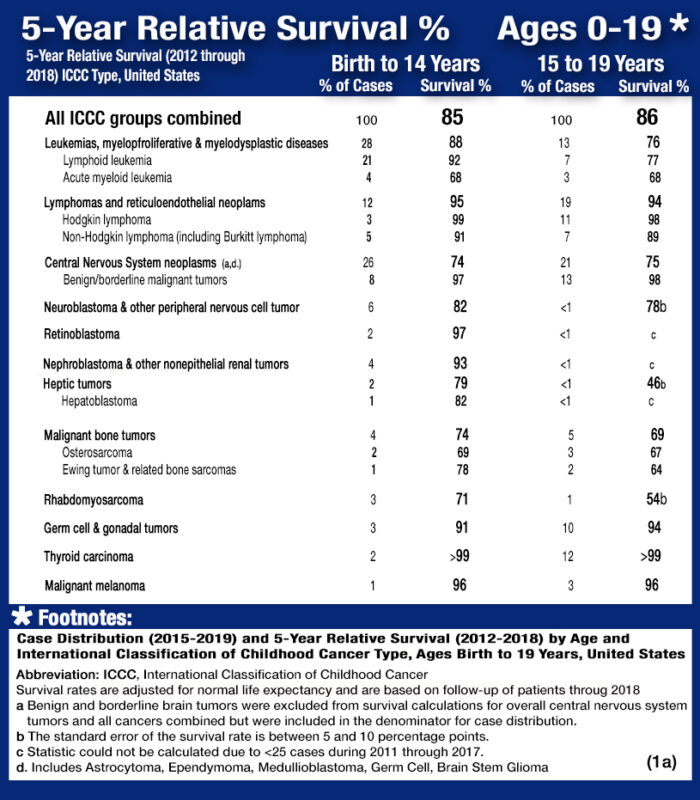
Survival
- The average 5-year survival rate for childhood cancer (Ages 0-19) as a whole is 86%. (1A)
- Cancer survival rates vary not only depending upon the type of cancer, but also upon individual factors attributable to each child. (6)Five year survival rates can range from almost 0% for cancers such as DIPG (2.2%(48)), a type of brain cancer, to over 90% for the most common type of childhood cancer known as Acute Lymphoma Leukemia (ALL). (1)
- Diffuse intrinsic pontine glioma (DIPG) represents approximately 80% of the malignant brainstem tumors occurring in children. (34)
- Despite numerous clinical trials, the outcome of children with DIPG continues to remain dismal, with a median survival of only 11 months, while only 10% of DIPG patients have ≥ 2-year overall survival (OS) rate. (48)
- As of January 1, 2018 (the most recent date for which data exist), approximately 483,000 survivors of childhood and adolescent cancer (diagnosed at ages 0 to 19 years) were alive in the United States. (37) The number of childhood cancer survivors is projected to grow to more than 500,000 by 2020. (27)
- Approximately 1 in 530 young adults aged 20 to 39, between is a survivor of childhood cancer. (1)
Pediatric Cancer 5-Year Ages 0 to 19 for years 2012 through 2018: The table below is a representation of the estimated 5-year survival rates for various types of childhood cancers. It should be noted the survival rates listed below reflect general rates and are in no way a representation of an anticipated actual survival outcome for any individual child.
Mortality
- Cancer is the number one cause of death by disease among children and adolescents in the USA. (1A)
- 1,040 children (aged 0 -14) and 550 adolescents (aged 15-19) are expected to die from cancer in 2023 (excluding benign and borderline malignant brain tumors). (1A)
- About 1 in 260 children and adolescents will be diagnosed with cancer before 20 years of age. (1A)
- Brain cancer represents 26% of total childhood cancer deaths while leukemia accounts for 28%.(1A)
- 1/3 of childhood brain and CNS cancers occur among those aged 5-9, median age at death is age 9. (7i)
- On average, about 14% of children die within 5 years of diagnosis.(1a) Among those children who survive to five years from diagnosis, 18% of them will die over the next 25 years. (50)
- Cancer death rates decreased an average of 0.9% per year among AYAs, and an average of 1.5% per year among children between 2015 and 2019. (7G)
- During 2001–2019, death rates among children (0-14) declined an average of 0.4% per year for brain and ONS cancer, whereas death rates from leukemia declined an average of 2.9% per year (7G)
- The most common causes of death in childhood cancer survivors are: The primary cancer comes back. A second (different) primary cancer forms. Heart and lung damage. (39)
- Those that survive the five years have an eight times greater mortality rate due to the increased risk of liver and heart disease and increased risk for reoccurrence of the original cancer or of a secondary cancer. (8)
- There are 69.3 potential life years lost on average when a child dies of cancer compared to 14 potential life years lost for adults. (13)
- Survivors of hereditary retinoblastoma, a rare cancer of the eye, have a high risk of developing subsequent cancers, particularly sarcomas of the soft tissue and bone. (73)
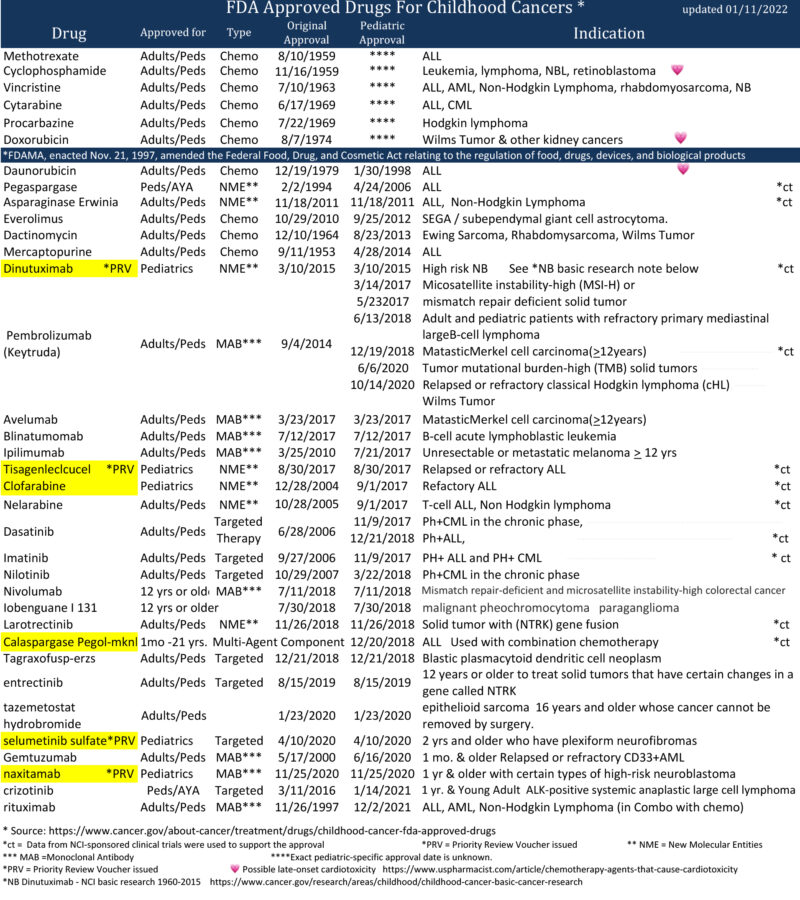
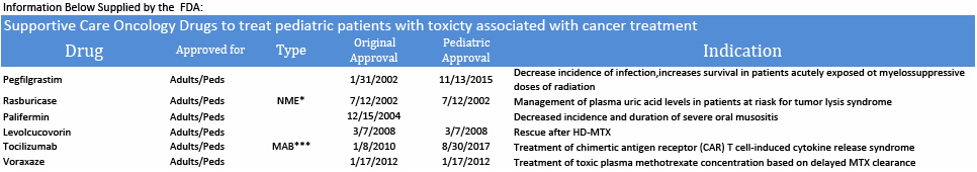
FDA Approved Drugs for Childhood Cancers
Highlighted drugs below were approved in the first instance for use in cancer treatment for children
Drug Development
- Between the years of 2009 and 2019, nine of the 11 drugs used to treat acute lymphoblastic leukemia — which is the most common childhood cancer — were in and out of shortage. (32)
- The median lag time from first-in-human to first-in-child trials of oncology agents that were ultimately approved by FDA was 6.5 years. (61)
- The FDA awarded Priority Review Vouchers (PRV) for four of the six drugs originally approved in the first instance for cancer treatment for children. PRV’s are transferable and are desired incentives for developers of drugs for rare pediatric diseases. Holders of a PRV get a faster FDA drug approval process for a future drug of their choice. The vouchers are transferable and may be sold or traded. (42)
- The US Congress created the priority review voucher program in 2007 based on a 2006 Health Affairs paper (Ridley et al. 2006). The voucher entitles the bearer to regulatory review in about six months rather than the standard ten months. The Food and Drug Administration (FDA) awards a voucher following approval of a treatment for a neglected disease, rare pediatric disease (Cancer is included in rare pediatric disease), or medical countermeasure. Two drugs receive priority review for each voucher: the drug winning a voucher for a neglected or rare pediatric disease and the drug using a voucher for another indication. (68)
The voucher may be sold. For example, a small company might win a voucher for developing a drug for a neglected disease, and sell the voucher to a large company for use on a commercial disease. Vouchers can sell for 100’s of millions of dollars. (68)

- While more than 200 cancer drugs have been developed and approved for adults,(58) the FDA, through March, 2023 has approved a total of 41 drugs for use in the treatment of childhood cancers. 35 of the drugs were originally approved only for adult use. Today we have only six drugs that were approved in the first instance for use in cancer treatment for children: Teniposide (1992 for ALL) use now discontinued by NCI, clofarabine (2004 for ALL), dinutuximab (2015 for NB), tisagenlecleucel (2017 for ALL), calaspargase pegol-mk (2018 for ALL), selumetinib (2020 for NF1) and naxitamab (2020 for NB). (7) In addition, the FDA has approved 7 drugs that help to reduce the toxicity associated with certain cancer treatments. (75)
Global Facts
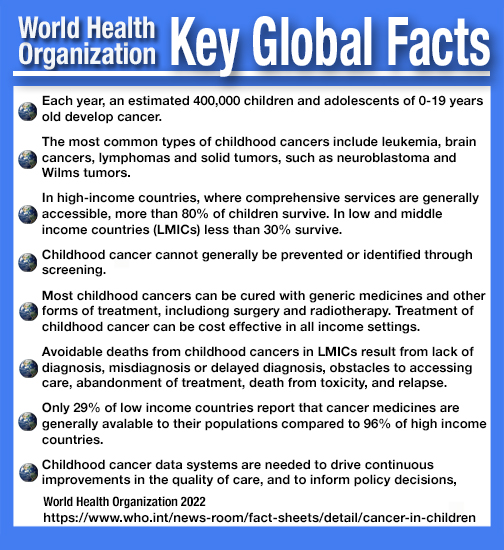
- Cancer kills more than 100,000 children each year. (33A)
- In Europe, since 1995, a total of 16 drugs have been approved for pediatric cancers. Seven of the 16 have been approved in the first instance specifically for pediatric cancers. Nine of the 16 were first approved for adults, then later for use in pediatric cancer. Eight of the total 16 drugs affected cancers responsible for less than 6% of all European childhood cancer deaths. (76)
- In 2018, The World Health Organization (WHO) launched the Global Initiative for Childhood Cancer with partners to provide leadership and technical assistance to support governments in building and sustaining high-quality childhood cancer programs. The goal is to achieve at least 60% survival rate globally by 2030, for all children with cancer. This represents an approximate doubling of the current cure rate and will save an additional one million lives over the next decade. The objectives are to increase capacity of countries to deliver best practices in childhood cancer care and also to prioritize childhood cancer and increase available funding at the national and global levels. (30)
- Some cancers are more prevalent in developing countries. For example, Burkitt’s lymphoma is more common in East and West Africa with over 4,000 cases in East Africa and over 10,000 in West Africa while only around 20 we recorded in the UK in 2015. (30)
Psychosocial Care (20)
- Childhood cancer threatens every aspect of the family’s life and the possibility of a future, which is why optimal cancer treatment must include psychosocial care. 11
- The provision of psychosocial care has been shown to yield better management of common disease-related symptoms and adverse effects of treatment such as pain and fatigue.12
- Depression and other psychosocial concerns can affect adherence to treatment regimens by impairing cognition, weakening motivation, and decreasing coping abilities. 13
- For children and families, treating the pain, symptoms, and stress of cancer enhances quality of life and is as important as treating the disease. 14
- Childhood cancer survivors reported higher rates of pain, fatigue, and sleep difficulties compared with siblings and peers, all of which are associated with poorer quality of life. 15
- Changes in routines disrupt day-to-day functioning of siblings .16 Siblings of children with cancer are at risk for emotional and behavioral difficulties, such as anxiety, depression, and post traumatic stress disorder.17
- Symptoms of posttraumatic stress disorder are well documented for parents whose children have completed cancer treatment. 18
- Chronic grief has been associated with many psychological (e.g., depression and anxiety) and somatic symptoms (e.g., loss of appetite, sleep disturbances, fatigue), including increased mortality risk. 19
- Cancer survivors in the United States reported medication use for anxiety and depression at rates nearly two times those reported by the general public, likely a reflection of greater emotional and physical burdens from cancer or its treatment. 21
- Financial hardship during childhood cancer has been found to affect a significant proportion of the population and to negatively impact family wellbeing. 22
- Adolescents with cancer experienced significantly more Health Related Hindrance (HRH) of personal goals than healthy peers, and their HRH was significantly associated with poorer health-related quality of life, negative affect, and depressive symptoms. 23
- Peer relationships of siblings of children with cancer are similar to classmates, though they experience small reductions in activity participation and school performance. 24
- Chronic health conditions resulting from childhood cancer therapies contribute to emotional distress in adult survivors. 25
- Parents have been found to report significant worsening of all their own health behaviors, including poorer diet and nutrition, decreased physical activity, and less time spent engaged in enjoyable activities 6 to 18 months following their child’s diagnosis. 26
Prevention
- Childhood cancer is fundamentally different to adult cancer in its biology, clinical classification, and treatment. Most childhood cancers are not caused by modifiable risk factors, public health campaigns would not have a large effect on decreasing their incidence (56)
- Over the past 50 years, the use of artificial chemicals in products has increased exponentially. Most of these chemicals were not tested for safety before widespread use, and the impacts of exposures are just now being realized. Children are especially vulnerable to the health impacts of chemical exposures, and these exposures are now known to be an important component of rising rates of diseases such as asthma, some cancers, and neurodevelopmental disorders in children.(74)
- Children are at an elevated risk for chronic disease because of increased exposure to environmental toxins. The U.S. Environmental Protection Agency (EPA) (2017) identifies children as uniquely vulnerable to environmental risks because of rapidly developing brains, lungs, immune and other bodily systems with less developed natural defenses than adults, including more permeable blood-brain barriers, and metabolic and detoxification pathways that are not yet fully developed.(74)
- Phthalates are a class of chemicals found in a variety of products. They are mixed with polyvinyl chloride and other plastics as a plasticizer that helps to make them soft and flexible. They are also added to cosmetics and other personal care products (often as a fragrance stabilizer), in medical equipment and coatings on medications, food production equipment and packaging, flooring, wall coverings, and other home products.(74) In a study of 1.3 million children aged under 19 years of age, childhood phthalate exposure was associated with incidence of osteosarcoma and lymphoma. (60, 60A)
- Pesticides are a group of chemicals intended to kill unwanted insects, plants, molds, and rodents, making them inherently toxic chemicals. Pesticides are not species-specific in their neurotoxic properties—a wanted effect on the nervous system of an insect can also be an unwanted effect on the nervous system of a child. (74) Exposures to pesticides, tobacco smoke, solvents, and traffic emissions have consistently demonstrated positive associations with risk of developing childhood leukemia.(53)
- Researchers found a higher level of common household pesticides in the urine of children with acute lymphoblastic leukemia. The findings should not be seen as cause-and-effect, but suggests an association between pesticide exposure and development of childhood ALL. (59)
- The U.S. Environmental Protection Agency (EPA) reports that 75 percent of U.S. households used at least one pesticide product indoors during the past year. The EPA also states, “Exposure to pesticides may result in irritation to eye, nose and throat, damage to central nervous system, kidney and increased risk of cancer.” (52)
- Exposure to toxic substances, such as industrial chemicals and radiation, can increase the risk of leukemia. People may encounter radiation during imaging tests such as MRI scans, X-rays, and CT scans.(57)
- Since children are more radiosensitive than adults and although CT scans are very useful clinically, potential cancer risks exist from associated ionizing radiation. (54)
- Exposure of parents to ionizing radiation is also a possible concern in terms of the development of cancer in their future offspring.. Children whose mothers had x-rays during pregnancy (that is children who were exposed before birth) and children exposed after birth to diagnostic medical radiation from computed tomography (CT) scans have been found to have a slight increase in risk of leukemia and brain tumors and possible other cancers. (37)
- Risk of childhood leukemia was associated with higher crop area near mother’s homes during pregnancy; CNS tumors were associated with higher cattle density. (51)
- Intake of vitamins and folate supplementation during the preconception period or pregnancy has been demonstrated to have a protective effect. (55)
Factors Affecting Follow Up Care
Stakeholders GAO interviewed and studies GAO reviewed identified three factors that affect access to follow-up care for childhood cancer survivors—individuals of any age who were diagnosed with cancer from ages 0 through 19. These factors are care affordability, survivors’ and health care providers’ knowledge of appropriate care, and proximity to care. Childhood cancer survivors need access to follow-up care over time for serious health effects known as late effects—such as developmental problems, heart conditions, and subsequent cancers—which result from their original cancer and its treatment.
- Affordability:Survivors of childhood cancer may have difficulty paying for follow-up care, which can affect their access to this care. For example, one study found that survivors were significantly more likely to have difficulty paying medical bills and delay medical care due to affordability concerns when compared to individuals with no history of cancer.
- Knowledge:Survivors’ access to appropriate follow-up care for late effects of childhood cancer can depend on both survivors’ and providers’ knowledge about such care, which can affect access in various ways, according to stakeholders GAO interviewed and studies GAO reviewed: (43)
- Some survivors may have been treated for cancer at an early age and may have limited awareness of the need for follow- up care.
- Some primary or specialty care providers may not be knowledgeable about guidelines for appropriate follow-up care, which can affect whether a survivor receives recommended treatment. Follow-up care may include psychosocial care (e.g., counseling), and palliative care (e.g., pain management).
- Proximity:Survivors may have difficulty reaching appropriate care settings. Stakeholders GAO interviewed and studies GAO reviewed noted that childhood cancer survivors may have to travel long distances to receive follow-up care from multidisciplinary outpatient clinics—referred to as childhood cancer survivorship clinics. The lack of proximity may make it particularly difficult for survivors with limited financial resources to adhere to recommended follow-up care.
Endnotes
1 American Cancer Society, Childhood and Adolescent Cancer Statistics, 2014
1A Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2023. CA: A Cancer Journal for Clinicians 2023; https://acsjournals.onlinelibrary.wiley.com/doi/full/10.3322/caac.21763
2 St. Jude Children’s Research Hospital, (JAMA. 2013:309 [22]: 2371-2381)
http://jama.jamanetwork.com/article.aspx?articleid=1696100
3 Lancet Oncology, Sep 2019 Volume 20 Number 9 p1211– p1225, “The global burden of childhood and adolescent cancer in 2017”
https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(19)30339-0/fulltext
4 National Vital Statistics Report, vol. 62.6, November 4, 2021
http://www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
5 Agency for Healthcare Research and Quality, US Dept. of Health & Human Services, “Pediatric Cancer Hospitalizations 2009, May 2012, Rebecca Anhang Price, Ph.D., Elizabeth Stranges, M.S., and Anne Elixhauser, Ph.D.
https://www.hcup-us.ahrq.gov/reports/statbriefs/sb132.jsp
6 American Society of Clinical Oncology
http://jco.ascopubs.org/content/28/15/2625.short
7 National Cancer Institute, http://www.cancer.gov/research/areas/childhood, December 20, 2022,
https://www.cancer.gov/research/areas/childhood/fda-approved-drugs-childhood-cancers?cid=eb_govdel
7A National Cancer Institute, “Age and Cancer Risk” 3/05/2021. Source: SEER 21 2013–2017, all races, both sexes.
https://www.cancer.gov/about-cancer/causes-prevention/risk/age
7B National Cancer Institute, SEER Cancer Statistics Review 1973-1997 (NCI 2000)
http://jnci.oxfordjournals.org/content/93/5/341.full
7C National Cancer Institute, NIH/NCI
https://fundedresearch.cancer.gov/nciportfolio/
7D National Cancer Institute, NIH/NCI
https://fundedresearch.cancer.gov/nciportfolio/about.jsp
7E Centers for Disease Control and Prevention, NCHS Data Brief No. 257, September 2016,“Declines in Cancer Death Rates Among Children and Adolescents in the United States, 1999-2014
https://www.cdc.gov/nchs/products/databriefs/db257.htm
7G Annual Report to the Nation 2022: Overall Cancer Statistics
https://seer.cancer.gov/report_to_nation/statistics.html#new
7i National Cancer Institute, SEER Percent of Deaths by Age, All races, Both Sexes
http://seer.cancer.gov/csr/2014_2018/results_merged/topic_med_age.pdf
8 Journal of the National Cancer Institute “Cause-Specific Late Mortality Among 5 Year Survivors”
http://jnci.oxfordjournals.org/content/100/19/1368.full
9 Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2018, National Cancer Institute. Bethesda, MD,
https://seer.cancer.gov/csr/1975_2018/, based on November 2020 SEER data submission, posted to the SEER web site, April 2021.
10 Additional information in this statement was obtained from several reliable and authoritative sources
11 Institute of Medicine, 2008 – Cancer Care for the Whole Patient
12 Jacobsen et al., 2012 (Journal of Clinical Oncology, 30 (11), p.1151-1153)
13 National Center for Health Statistics (NCHS): National Vital Statistics System (NVSS) “Provisional Life Expectancy Estimates for January through June, 2020, Report #10, Feb. 2021
https://www.cdc.gov/nchs/data/vsrr/VSRR10-508.pdf
14 Institute of Medicine 2015 – Comprehensive Care for Children with Cancer and Their Families
15 Children’s Oncology Group Long Term Follow-Up Guidelines, 2013
16 Alderfer et al., 2010 (Psycho-oncology, 19 (8), p. 789-805)
17 Alderfer et al., 2003 (Journal of Pediatric Psychology, 28 (4), p. 281-286)
18 Kazak et al., 2004 (Journal of Pediatric Psychology, 29 (3), p. 211-219)
19 Alam et al., 2012 (Death Studies, 36 (1), p. 1-22)
20 Psychosocial care addresses the effects that cancer treatment has on the mental health and emotional wellbeing of patients, their family members, and their professional caregivers. A single profession alone does not provide psychosocial care: Instead, every patient-healthcare provider interaction provides an opportunity to assess the stressors and concerns of children and their family members.
21 Hawkins et al., 2017 (Journal of Clinical Oncology, 5 (1), 78-87)
22 Bona et al., 2014 (Journal of Pain Symptom Management, 47 (3), 594-600)
23 Schwartz & Brumley, 2017 (Journal of Adolescent & Young Adult Oncology, 6 (1), 142-149)
24 Alderfer et al., 2015 (Journal of Pediatric Psychology, 40 (3) 309–319)
25 Vuotto et al., 2017 (Cancer, 123 (3), 521-528)
26 Wiener et al., 2016 (Journal of Pediatric Oncology Nursing, 33(5), 378–386)
27 Robison LL, Hudson MM. Survivors of childhood & adolescent cancer: life long risks & responsibilities. Nat Rev Cancer 22014; 14:6170 NCI
https://www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
28 UChicagoMedicine Understanding risks for childhood cancer survivors
29 Kebudi, R. and F.B. Cakir, Management of Diffuse Pontine Gliomas in Children: Recent Developments. Pediatric Drugs, 2013. 15(5): 351-362
30 World Health Organization
https://www.who.int/news-room/fact-sheets/detail/cancer-in-children
30A World Health Organization
https://www.who.int/cancer/childhood-cancer/en/
30b World Health Organization 2021 Dec. 13, “Childhood Cancer: Key Facts,”
https://www.who.int/news-room/fact-sheets/detail/cancer-in-children
31 The Lancet. Science Daily, 26 February 2019.
www.sciencedaily.com/releases/2019/02/190226184140
32 FDA Report Drug Shortages
https://www.fda.gov/drugs/drug-shortages/report-drug-shortages-root-causes-and-potential-solutions
33 Lancet Oncology. 2015 Mar; 16(3): e123–e136. doi: 10.1016/S1470- 2045(14)70409-7
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4485458/
33A Lancet Oncology. “Sustainable care for children with cancer.” 03/30/2020
https://www.thelancet.com/commissions/childhood-cancer
34 Effect of Time from Diagnosis to Start of Radiotherapy on Children with Diffuse Intrinsic Pontine Glioma 2014 Jan 30. doi: 10.1002/pbc.24971 PMCID: PMC4378861NIHMSID: NIHMS667729 PMID: 24482196
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378861/
35 Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death 1999- 2019 on CDC WONDER Online Database, released in 2020. Data are from the Multiple Cause of Death Files, 1999-2019, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program.
http://wonder.cdc.gov/ucd-icd10.html
36 The National Children’s Cancer Society, The Economic Impact of Childhood Cancer, November 30, 2018
Retrieved from https://policycommons.net/artifacts/1647909/the-economic-impact-of-childhood-cancer/ on 16Dec 2021. CID:20.500.12592/qp3g3v.
36a Household income and risk-of-poverty of parents of long-term childhood cancer survivors, Pediatric Blood Cancer, 2017 Aug;64(8).doi: 10.1002/pbc.26456. Epub 2017 Mar 6.
https://pubmed.ncbi.nlm.nih.gov/28266129/
37 The National Cancer Institute “Cancer in Children and Adolescents” 11/04/2021
https://www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
38 American Cancer Society, Treatment and Survivorship Statistics, 2019
https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21565
39 National Cancer Institute, NIH/NCI Late Effects of Treatment for Childhood Cancer (PDQ®)–Patient Version
https://www.cancer.gov/types/childhood-cancers/late-effects-pdq
40 National Cancer Institute, Cancer Stat Facts: Cancer Among Adolescents and Young Adults (AYAs) (Ages 15–39)
https://seer.cancer.gov/statfacts/html/aya.html
41 U.S. News & World Reports “Childhood Cancer Survivors Still Face Shorter Life Expectancy,” January 2,2020
42 Food and Drug Administration, FDA, 12,27,2020, Rare Pediatric Disease (RPD) Designation and Voucher Programs
43 United States Government Accounting Offices, GAO-20-636R, Jul 31, 2020. “Survivors of Childhood Cancer: Factors Affecting Access to Follow-up Care”
https://www.gao.gov/products/gao-20-636r
44 Cancer Epidemiology, ”Childhood cancer: Estimating regional and global incidence,” Volume 71, Part B, April 2021, 101662, Used 3.4 2015 Global Childhood Cancer (GCC) Model
https://www.sciencedirect.com/science/article/pii/S1877782119301729
45 NIH/National Cancer Institute, Age-Adjusted and Age-Specific SEER Cancer Incidence Rates, 2014-2018, Table 2.1
https://seer.cancer.gov/csr/1975_2018/results_single/sect_02_table.01_2pgs.pdf
45A NIH/National Cancer Institute, Age-Adjusted and Age-Specific SEER Cancer Incidence Rates, 2014-2018, Table 2.4
https://seer.cancer.gov/csr/1975_2018/results_single/sect_02_table.01_2pgs.pdf
46 Lancet Oncology, Volume 20, Issue 7, July 2019, Pages 972-983, “Global childhood cancer survival estimates and priority- setting: a simulation-based analysis,”
https://www.sciencedirect.com/science/article/abs/pii/S1470204519302736
47 Cancer Epidemiology Biomarkers, 1 August 2021, DOI:10.1158/1055-9965.EPI-21-0154
48 Hofmann et al. (J Clin Oncol, 2018 vol. 36(19) pp. 1963-1972)
https://pubmed.ncbi.nlm.nih.gov/29746225/
49 National Cancer Institute Illustration by Cristiana Couciero May 16, 2016
50 New England Journal of Medicine, Armstrong GT, Chen Y, Yasui Y, et al. Reduction in late mortality among 5-year survivors of childhood cancer. N Engl J Med. 2016;374:833-842.
https://www.nejm.org/doi/10.1056/NEJMoa1510795
51 Residential proximity to agriculture and risk of childhood leukemia and central nervous system tumors in the Danish national birth cohort.
https://pubmed.ncbi.nlm.nih.gov/32711331/
52 US Environmental Protection Agency. Pesticides and Child Safety. Washington, DC: US Environmental Protection Agency; “Pesticides’ Impact on Indoor Air Quality,”
https://www.epa.gov/indoor-air-quality-iaq/pesticides-impact-indoor-air-quality
53 Science Digest. “Current Problems in Pediatric and Adolescent Health Care,” Volume 46, Issue 10, October 2016, Pages 317-352,
https://www.sciencedirect.com/science/article/pii/S1538544216300694
54 Lancet. 2012 Aug 4;380(9840):499-505. doi: 10.1016/S0140-6736(12)60815-0.Epub 2012 Jun 7. “Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study,” PubMed
https://pubmed.ncbi.nlm.nih.gov/22681860/
55 American Academy of Pediatrics, “Childhood Leukemia: A Preventable Disease,” Volume 138, Issue Supplement_1, November 2016,
56 The Lancet. 4/1/2020 Volume 21Number 4, p.489, “Sustainable care for indigenous children with cancer.”
https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(20)30137-6/fulltext
57 Medical News Today, “Is leukemia hereditary?” by Jamie Eske, May 30, 2019
https://www.medicalnewstoday.com/articles/325332
58 JAMA Network 3/15/2022 Volume 5 Number 3, doi:10.1001/jamanetworkopen.2022.2265. “Cancer Drug Approvals That Displaced Existing Standard-of-Care Therapies, 2016-2021,” David J. Benjamin, MD; Alexander Xu, BA; Mark P. Lythgoe, MBBS; et al
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2790102
59 Georgetown University Medical Center “Common Household Pesticides Linked To Childhood Cancer Cases In Washington Area”: August 4, 2009,
https://www.sciencedaily.com/releases/2009/07/090728102306.htm
60 CTVNews, HEALTH News, 3/18/2022, “Exposure to ‘everyday chemical’ associated with higher incidence of childhood cancer: study, Journal of the National Cancer Institute 2/18/2022:
https://pubmed.ncbi.nlm.nih.gov/35179607/
61 European Journal of Cancer, Volume 112 pg 49-56, May 1, 2019 , “Timing of first-in-child trials of FDA-approved oncology drugs.” Dylan V, Neel, David S. Shulman, Steven G. DuBois. Published March 28, 2019, DOI:
https://doi.org/10.1016/j.ejca.2019.02.011
62 Hsu T-W, Liang C-S, Tsai S-J, et al. Risk of major psychiatric disorders among children and adolescents surviving malignancies: A nationwide longitudinal study.
https://ascopubs.org/doi/abs/10.1200/JCO.22.01189 J Clin Oncol. Published online January 17, 2023. doi:10.1200/JCO.22.01189
63 National Cancer Institute, “Cancer in Children and Adolescents,” November 4, 2021,
64 Hudson MM. Reproductive outcomes for survivors of childhood cancer. Obstet Gynecol. 2010 Nov;116(5):1171-83. doi: 10.1097/AOG.0b013e3181f87c4b. PMID: 20966703; PMCID: PMC4729296.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4729296/
65 World Health Organization, 04 February 2023, World Cancer Day 2023, Message of the WHO Regional Director for Africa, Dr Matshidiso Moeti
https://www.afro.who.int/regional-director/speeches-messages/world-cancer-day-2023
66 American Cancer Society, How Cancer and Cancer Treatment Can Affect Fertility in Females, “Bone marrow or stem cell transplant,”: Page 7
67 National Brain Tumor Society, Brain Tumor Facts, Brain Tumors in All Pediatric Populations (0-19)
68 Duke University, Fuqua School of Business, Dr. David Ridley, Dr. and Mrs. Frank A. Riddick, Priority Review Vouchers, Home Website, Overview:
https://sites.fuqua.duke.edu/priorityreviewvoucher/
69 The Lancet. Oncology, January, 2022, VOLUME 23, ISSUE 1, P27-52, The global burden of adolescent and young adult cancer in 2019: a systematic analysis for the Global Burden of Disease Study 2019
https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(21)00581-7/fulltext
70 The Lancet. Oncology, September 2019, Volume 20, Issue 9, Pages 1211-1225, The global burden of childhood and adolescent cancer in 2017: an analysis of the Global Burden of Disease Study
https://www.sciencedirect.com/journal/the-lancet-oncology/vol/20/issue/9
71 World Health Organization, WHO Regional Director for Africa, Dr Matshidiso Moeti, 04 February 2023 Message, 771
https://www.afro.who.int/regional-director/speeches-messages/world-cancer-day-2023
72 National Cancer Institute, Division of Cancer Epidemiology & Genetics: Increased Meningioma Risk Following Treatments for Childhood Cancer
https://dceg.cancer.gov/news-events/news/2022/meningioma-risk-childhood-cancer
73 National Cancer Institute, Division of Cancer Epidemiology & Genetics: February 11, 2021, Subsequent Cancer Risk in Retinoblastoma Survivors
https://dceg.cancer.gov/news-events/news/2021/retinoblastoma-subsequent-cancer-risk
74 Journal of Pediatric Health Care, Pediatric Chemical Exposure: Opportunities for Prevention Volume 36, Issue 1, January–February 2022, Pages 27-33
https://www.sciencedirect.com/science/article/abs/pii/S0891524521002194
75 U.S. Food and Drug Administration, Approved Drugs, December 20, 2022
https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm
THIS DOCUMENT IS NOT INTENDED TO OFFER SPECIFIC STATISTICS REGARDING AN INDIVIDUAL PATIENT OR THE PATIENT’S SPECIFIC FORM OF CANCER AND IS NOT A SUBSTITUTE FOR INFORMATION THAT MAY BE SOUGHT FROM A PHYSICIAN. IT IS MERELY INTENDED, BASED ON INFORMATION PRESENTLY AVAILABLE TO THE AUTHORS, TO BE A GOOD FAITH GENERAL PRESENTATION OF CHILDHOOD CANCER STATISTICS THAT MAY BE HELPFUL TO OTHERS SEEKING SUCH GENERAL INFORMATION.
June 30, 2023